1. Introduction
The Coronavirus of 2019 (COVID-19) pandemic—which exceeded 6.96 million deaths globally as of October 2023 (
World Health Organization 2023)—highlighted the importance of social behaviour and compliance with public health restrictions in determining an individual’s probability of contracting a communicable disease. Reducing contacts with others through physical distancing and refraining from attending large gatherings were shown to dramatically reduce the transmission of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19 (
Lewnard and Lo 2020;
Quilty et al. 2020;
Champredon et al. 2021). Raising public awareness of factors that contribute to disease spread and quantifying the personal risk of being exposed to diseases could encourage compliance with government policies aimed at mitigating transmission. Suitable risk assessment and communication tools could facilitate knowledge translation and inform policy decisions with respect to managing communicable disease transmission (
Chatterjee et al. 2020).
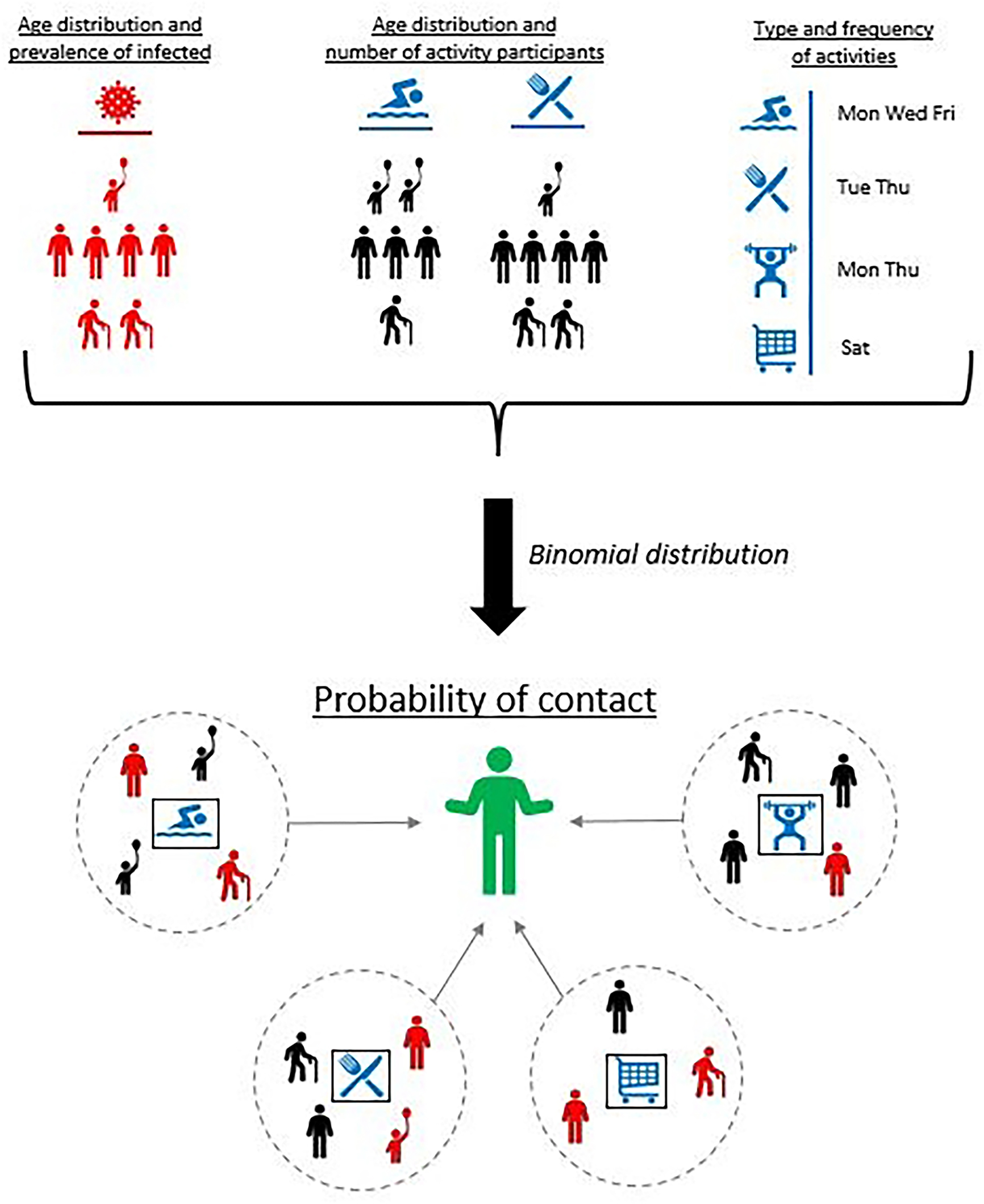
We designed a model to provide decision makers with information on the potential effectiveness of targeted behavioural restrictions. Our model estimates an individual’s probability of physically contacting an infected person as a function of the prevalence in their location and of the (likely multiple) activities in which they engaged in the 14 days prior to the date of assessment. Age of activity participants plays a crucial role in determining contact patterns, and accounting for age-dependent contact patterns is essential when considering the spread of COVID-19 in non-household settings (
Davies et al. 2020). However, the context of the contacts is also important. Consider the probability of contact within a bar: in some jurisdictions, children are not allowed, so this not only means contact with an infected child should not be possible, but the general behavioural correlations between children and adults (i.e., children and their caretakers) would not apply to this activity.
A comparable model is the COVID-19 Missed Infection Calculator developed by Defence Research and Development Canada (DRDC) for the Canadian Armed Forces (
Guillouzic et al. 2022), which estimates the probability of one or more individuals with undetected infections being in a group. The calculator has the added complexity of accounting for quarantining and testing practices, though it treats each member of the group as coming from a homogeneous population. In contrast, our contact probability model predicts the probability of contact (rather than infection) over multiple activities, and accounts for demographic differences among group members and the population.
The Public Health Agency of Canada (PHAC) Gathering Risks Model: On-line calculator (
Champredon et al. 2021) uses a mathematically similar approach to the contact model to quantify the likelihood that an infectious individual is present at a gathering. The PHAC model recommends using the relative risk of infection for participants compared to the population to account for population heterogeneity. Our contact probability model includes a similar modification through the inclusion of an age adjustment factor (described below) but predicts the probability of contact with an infected person, and accounts for prior behaviours leading up to the grouping event.
3. Example scenarios
Policymakers, as part of their decision-making process, may be interested in understanding the impact of different activities when deciding whether restrictions should be applied with the overall goal of controlling a communicable disease. This information would be considered alongside other effects, such as the impact on citizens’ personal freedoms and the need to prevent healthcare systems from collapsing, as was seen in the early days of the COVID-19 pandemic.
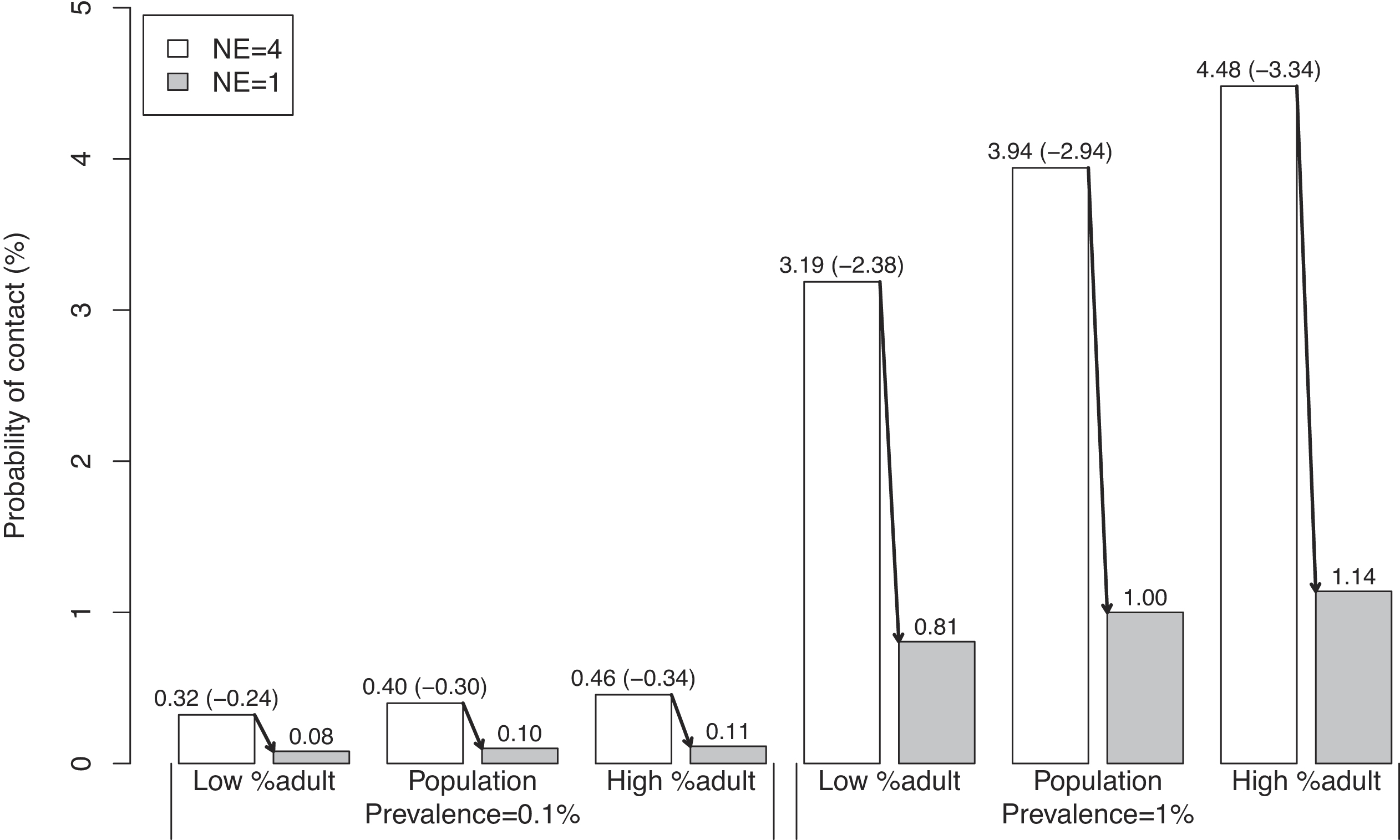
Section 4 presents two scenarios related to this. The first one, in
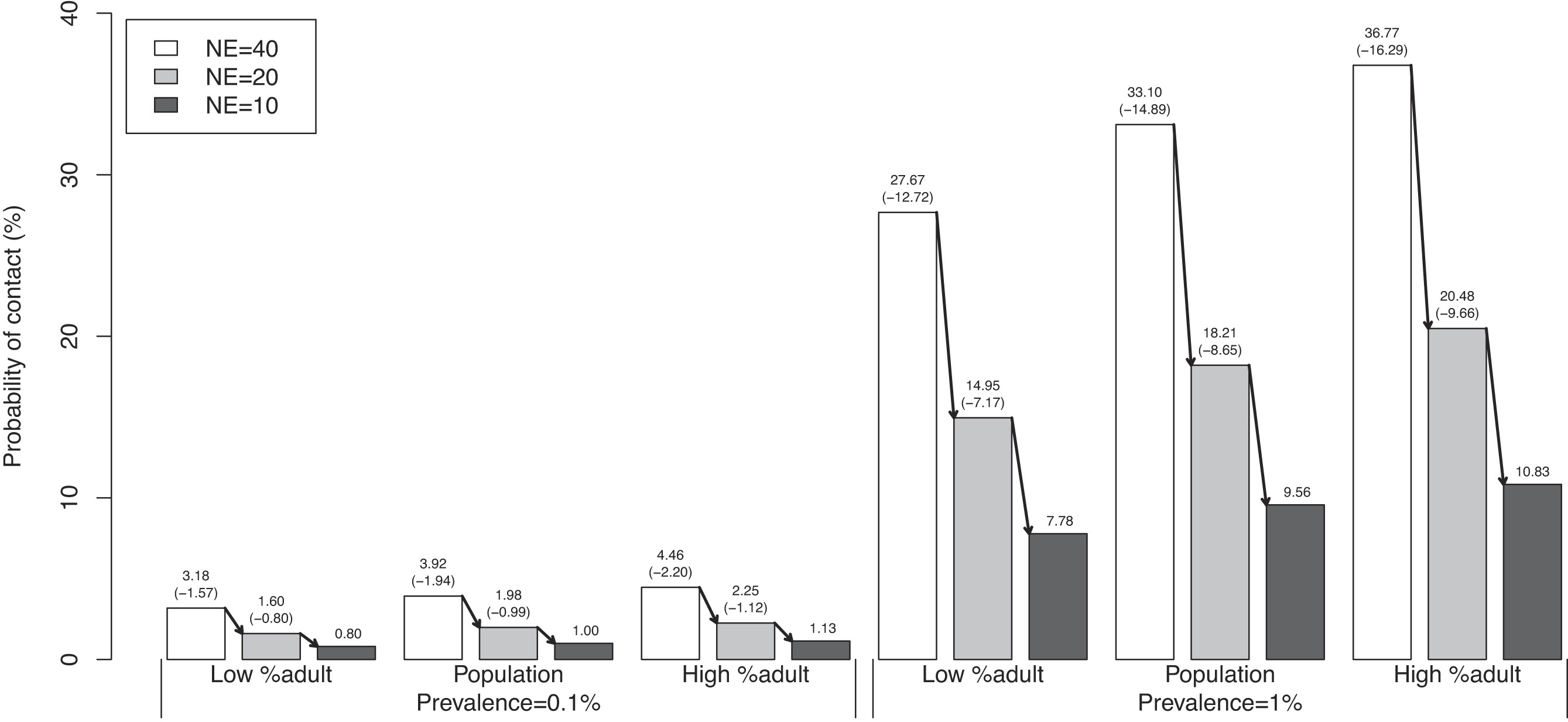
Section 4.2, relates to capacity restrictions on restaurants. The second one, in
Section 4.3, demonstrates how the contact model could inform a decision maker on the impact that restricting a range of various activities could have on the total probability of contact. The scenarios utilize and compare three different age distributions: "Population" refers to the age distribution of the 2020 Yukon population, "Low %adult" assigns 25% of activity participants to adults with the remainder distributed to other age categories proportional to the Yukon population, and "High %adult" assigns 80% of activity participants to adults with the remainder distributed to other age categories proportional to the Yukon population. Variations in the activity age distribution were focused on the adult age category because it had the highest proportion of known infections, and hence would have the largest impact on the results.
For the second scenario, we used a pre-pandemic transportation survey done in Kingston, Ontario (
R.A. Malatest and Associates Ltd. 2019) that provided a count of activity participants, a list of activities performed, the relative likelihood of performing those activities, and the mean number of activities performed per day. We subsetted the list of potential activities provided in the Kingston report to include shopping, personal, dining, recreation, and work. We used the sample values in
Table 1 for shopping and dining, and equated “healthcare” and “gym” in
Table 1 to the “personal” and “recreation” activities in the Kingston report.
We used
eqs. 1–
7 to create an age adjustment factor and probability of contact for the “work” activity that did not appear in
Table 1. The 2021 census (
Statistics Canada 2022) was used to create the age distribution for the Kingston population. People aged 20–59 years were assumed to make up 90% of activity participants, with 5% in each of the 0–20 and 60–69-year-old age categories. The age distribution of infections was assumed to be the same as in
Section 2.3, which led to an age adjustment factor of 1.29. Assuming a prevalence of 1% and a small office setting of approximately five encounters during the day, the daily contact probability was 6.3% for the new “work” activity.
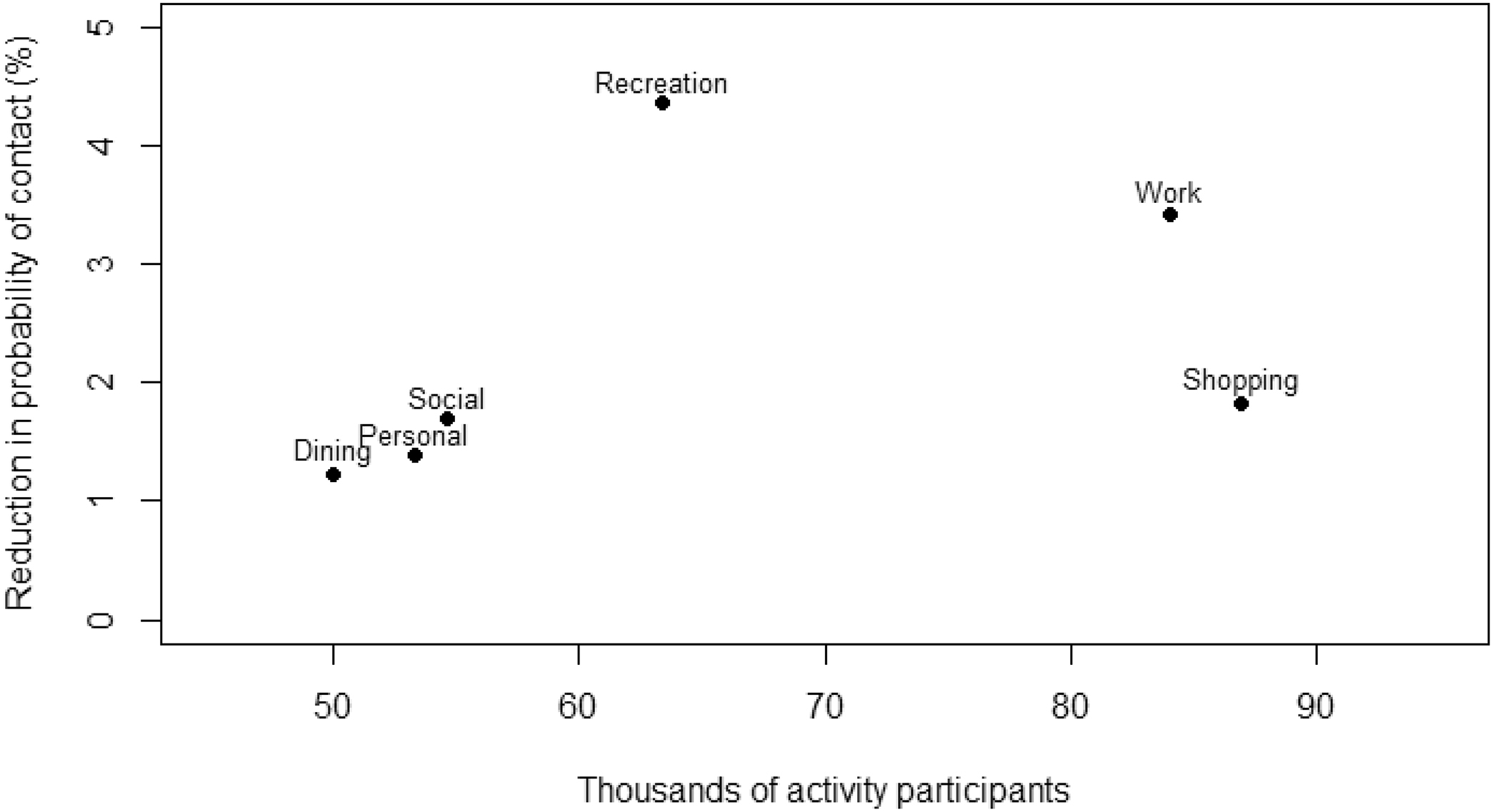
A simulation was used to examine the impact of reducing each of the five activities in turn. Each of the Kingston residents was assumed to do a number of activities drawn from a Poisson distribution with a mean of 2.98 (the mean number of activities stated in the Kingston report). Individuals assigned more than five activities from the random draw were treated as if they participated in five activities. The specific activities performed by an individual were then selected randomly from the list of activities considered, based on the relative frequency provided in the Kingston survey. People were not allowed to perform the same activity twice in the simulation since it covered a single day. The probability of contact for each individual’s set of activities was calculated using
eq. 8, and the mean probability of contact across the whole population was recorded.
Afterwards, the probability of contact for a given activity was set to zero to mimic the effect of restricting that activity, and the simulation rerun. (We did not want to increase the probability of doing other activities due to an activity restriction, so the probability of contact was manually set to zero instead of the probability of performing the activity.) The mean probability of contact across the whole population excluding the restricted activity was calculated and repeated for each restricted activity.
5. Discussion
The COVID-19 pandemic highlighted the importance of managing social behaviours that encourage disease spread. During the initial stages of the pandemic, there was a significant amount of ambiguity regarding the data accessible for determining the appropriate public health measures to implement and their execution strategies. As such, assumptions were made about social behaviours, activity group sizes, and the eventual effect of these public health measures on reducing the number of cases in the community. Our contact model is applicable to assessing the impacts of within-jurisdiction health measures on the probability of contacting infectious individuals. In particular, it can be used to estimate the impact of the disparity in prevalence among age groups on the reduction that can be expected from group-size restrictions. As a follow up to this research, the probability of contact obtained from this contact model could be used as input to other models that consider transmission, such as compartmental models or a statistical model to calculate the probability of transmission given the probability of contact.
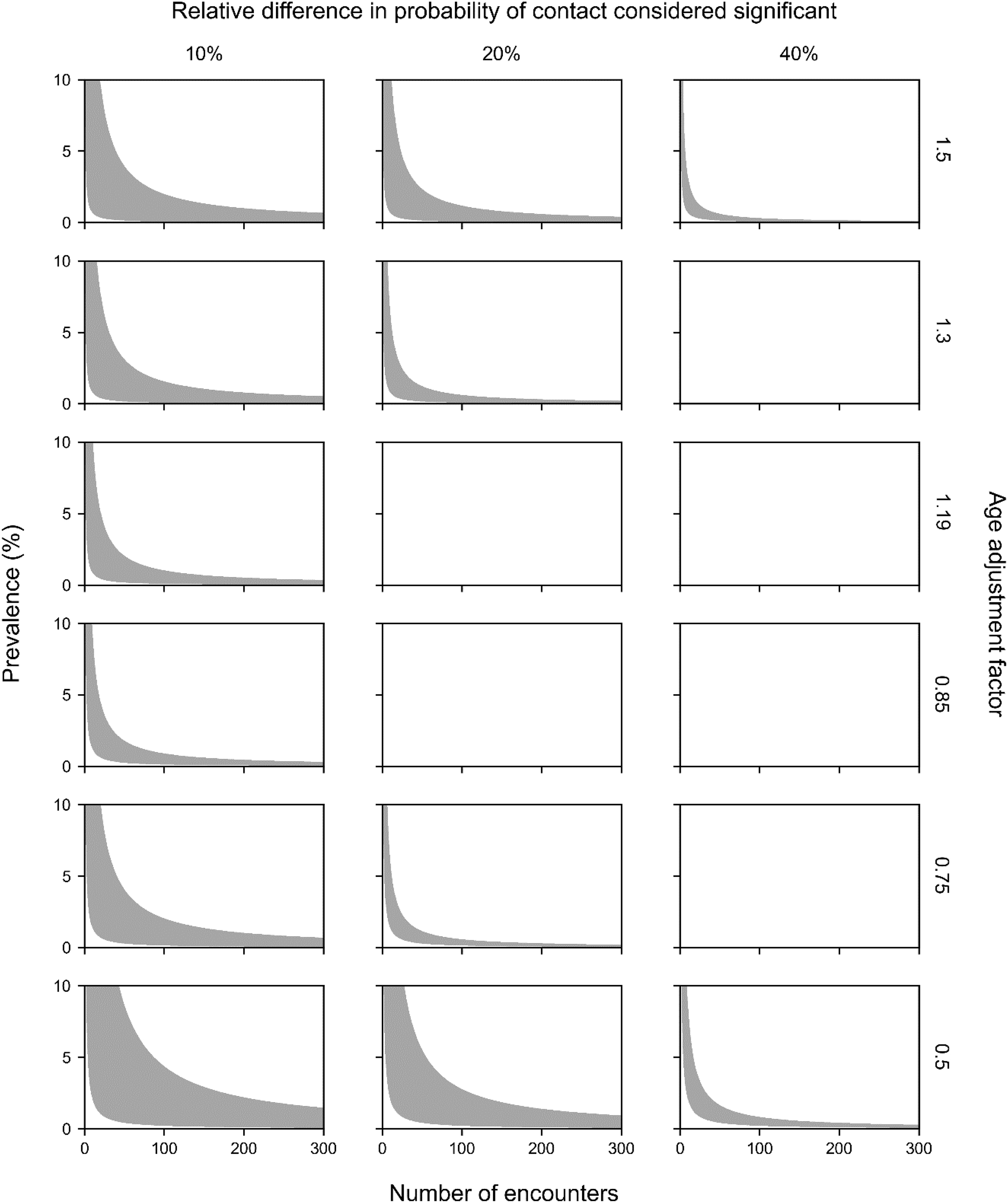
Applications of our model demonstrate that the impact of age distribution on the probability of contact can be substantial for intermediate values of prevalence and groups sizes when there is a sufficiently large difference in prevalence between age groups. The age adjustment factor produced differences of up to 20% in the probability of contact under realistic activity age distributions. However, when the prevalence was small, the age adjustment factor had a minor effect on the probability of contact, because the probability of contact was and remained small. At the other extreme, when the prevalence or group sizes were large, the overall probabilities of contact were close to one and the impact of the age adjustment factor was also negligible. The age adjustment factor could play an important role in estimating the probability of contact when there is a disparity in infection rates between various age groups, and the prevalence and number of encounters assume intermediate values. The concept of an age adjustment factor could be extended to account for differences in prevalence among other subpopulations such as occupation groups and vaccination status.
The contact model considered group members to be randomly chosen from age-specific subpopulations. This simplifying assumption, common to importation models (e.g.,
Champredon et al. 2021), ignores correlations between the infection status of cohorting individuals. One type of age cohorting is addressed through our contact model’s activity age adjustment factor: this corrects for different proportions of age groups participating in each activity. The model does not address the non-random cohorting expected to occur in each group. For instance, when participating in a seated dining activity, people are more likely to sit with others with whom they have repeated exposure, such as family members and friends. The repeated exposure imposes a correlation in infection status among the group members. This could be addressed in the contact model by replacing the number of people encountered in an activity by the number of cohorts encountered at that activity. This correction is related to the public health policy of “bubbling”, where the number of unique contacts is limited to the people in your bubble.
Since each activity contributes to a person’s total probability of contact, it is important to correctly identify the list of activities a person can do. In the activity restriction example, we subsetted the list of activities to those where the Kingston transportation survey and
Table 1 had reasonable overlap. If using the contact model for decision-making, a more comprehensive list of activities may need to be compiled.
Like all models, the results of our contact probability model are limited by the accuracy of the parameters.
Table 1 presents sample values for group sizes and age distributions of people participating in different activities, but limited data were available. Travel surveys, such as the one used in the activity restriction scenario, are available from many cities and may contain useful behaviour data. Other surveys that quantify activity participation could also provide invaluable information. However, behaviours early in the COVID-19 pandemic differed from normal behaviours and evolved throughout the pandemic because of policies, vaccines, and habituation. Before using the contact model for policy decisions, a decision maker should consider the following:
•
How many people are in a community?
•
What activities in the community involve people contacting people outside their household?
•
How many people participate in those activities?
•
How many different groups of people participate in a given activity?
•
What is the age distribution of activity participants?
•
What is the local infectious disease prevalence?
•
What is the age distribution of the infectious disease prevalence?
This is an extensive list of questions that may not be readily answered, especially if time-sensitive decisions need to be made. To address data limitations in future studies, we suggest deploying observers to an assortment of locations to record approximate group sizes and ages, which could provide further validity. Such visual surveys could be done quickly, remotely (no interaction with activity participants being required), and repeatably. A visual survey would also avoid reporting biases that likely exist when people are asked to report their behaviours in a written survey, especially when public health measures encourage limiting group sizes or activities. Visual surveys would ideally be supplemented by interviews to provide information about cohorting, and other activities in which a person engaged that were not directly observed. Alternative approaches, including collecting microcontact data through cellular phones, could also be deployed to support modelling efforts (for a past example during the H1N1 pandemic, see
Hashemian et al. (2012)).